What Is The Soap Format In A Medical Record . soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method for documenting patient information in healthcare. documenting a patient assessment in the notes is something all medical students need to practice. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. This section includes the patient's. soap is an acronym that stands for subjective, objective, assessment, and plan.
from www.examples.com
soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. documenting a patient assessment in the notes is something all medical students need to practice. This section includes the patient's. soap is an acronym that stands for subjective, objective, assessment, and plan. soap notes are a standardized method for documenting patient information in healthcare. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients.
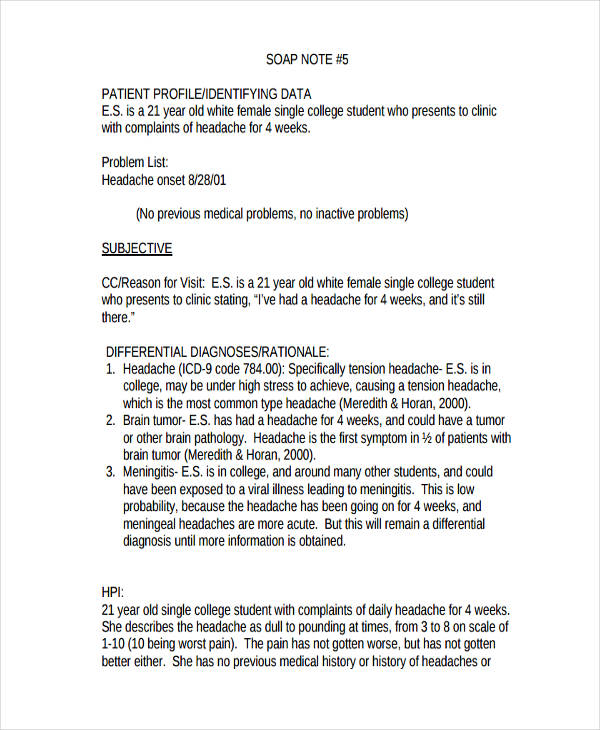
SOAP Note 19+ Examples, Format, How to Write, PDF
What Is The Soap Format In A Medical Record soap is an acronym that stands for subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap is an acronym that stands for subjective, objective, assessment, and plan. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a standardized method for documenting patient information in healthcare. This section includes the patient's.
From www.researchgate.net
An example progress note with SOAP sections annotated. Line breaks are What Is The Soap Format In A Medical Record This section includes the patient's. soap is an acronym that stands for subjective, objective, assessment, and plan. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. learn how to write a soap note. What Is The Soap Format In A Medical Record.
From www.unihomeworkhelp.com
Complete Guide to Understanding SOAP Notes Unihomework Help What Is The Soap Format In A Medical Record soap notes are a standardized method for documenting patient information in healthcare. This section includes the patient's. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. documenting a patient assessment in the notes is something all medical students need to practice. soap is an acronym that stands for. What Is The Soap Format In A Medical Record.
From www.process.st
SOAP Note How to Write Spotless Healthcare Notes (Free Template What Is The Soap Format In A Medical Record soap is an acronym that stands for subjective, objective, assessment, and plan. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a. What Is The Soap Format In A Medical Record.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is The Soap Format In A Medical Record soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap is an acronym that stands for subjective, objective, assessment, and plan. This section includes the patient's. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap—or subjective, objective, assessment and plan—notes allow. What Is The Soap Format In A Medical Record.
From www.allbusinesstemplates.com
Medical Soapnote Templates at What Is The Soap Format In A Medical Record soap notes are a standardized method for documenting patient information in healthcare. soap is an acronym that stands for subjective, objective, assessment, and plan. documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or. What Is The Soap Format In A Medical Record.
From positivepsychology.com
What are SOAP Notes in Counseling? (+ Examples) What Is The Soap Format In A Medical Record soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. This section includes the patient's. soap notes are a. What Is The Soap Format In A Medical Record.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates ᐅ TemplateLab What Is The Soap Format In A Medical Record soap notes are a standardized method for documenting patient information in healthcare. soap is an acronym that stands for subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings.. What Is The Soap Format In A Medical Record.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is The Soap Format In A Medical Record soap is an acronym that stands for subjective, objective, assessment, and plan. This section includes the patient's. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes are a standardized method for documenting patient information in healthcare. soap notes are a standardized method of documenting patient encounters. What Is The Soap Format In A Medical Record.
From ceevecbr.blob.core.windows.net
What Is Soap In Medical School at Jerry Harper blog What Is The Soap Format In A Medical Record documenting a patient assessment in the notes is something all medical students need to practice. This section includes the patient's. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap is an acronym that stands for subjective, objective, assessment, and plan. soap—or subjective, objective, assessment and plan—notes allow. What Is The Soap Format In A Medical Record.
From www.pinterest.com
Example of SOAP Note Soap note, Notes template, Medical history What Is The Soap Format In A Medical Record soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. documenting a patient assessment in the notes is something all medical students need to practice. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method for documenting patient. What Is The Soap Format In A Medical Record.
From www.pinterest.com
Soap Report Template in 2023 Soap note, Notes template, Nurse study notes What Is The Soap Format In A Medical Record soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. learn how to write a soap note so you can efficiently track,. What Is The Soap Format In A Medical Record.
From medium.com
What is a Soap Note. According to Physiopedia SOAP notes are… by What Is The Soap Format In A Medical Record soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap is an acronym that stands for. What Is The Soap Format In A Medical Record.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is The Soap Format In A Medical Record learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or subjective, objective, assessment and plan—notes allow clinicians to. What Is The Soap Format In A Medical Record.
From www.template.net
11+ Soap Note Templates Free Sample, Example, Format Download! What Is The Soap Format In A Medical Record soap notes are a standardized method for documenting patient information in healthcare. soap is an acronym that stands for subjective, objective, assessment, and plan. documenting a patient assessment in the notes is something all medical students need to practice. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients.. What Is The Soap Format In A Medical Record.
From dxorhmyma.blob.core.windows.net
What Is A Soap In Medical Terms at Gretchen Price blog What Is The Soap Format In A Medical Record soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. This section includes the patient's. learn how to write a soap note. What Is The Soap Format In A Medical Record.
From www.examples.com
SOAP Note 19+ Examples, Format, How to Write, PDF What Is The Soap Format In A Medical Record learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes are a standardized method of documenting patient encounters in medical and healthcare settings. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method for. What Is The Soap Format In A Medical Record.
From studylib.net
Patient SOAP Note Charting Procedures What Is The Soap Format In A Medical Record documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a standardized method for documenting patient information in healthcare. soap—or subjective, objective, assessment and plan—notes allow clinicians to document continuing patient encounters in a structured way. soap notes are a standardized method of documenting patient encounters in medical. What Is The Soap Format In A Medical Record.
From templatelab.com
40 Fantastic SOAP Note Examples & Templates Template Lab What Is The Soap Format In A Medical Record documenting a patient assessment in the notes is something all medical students need to practice. soap notes are a standardized method for documenting patient information in healthcare. This section includes the patient's. learn how to write a soap note so you can efficiently track, assess, diagnose, and treat clients. soap notes are a standardized method of. What Is The Soap Format In A Medical Record.